Dendritic Ulcer Causes and Prevention in Herpes Eye Infections
Dr. Krishna Vaitheeswaran
Standard advice about corneal infections often lumps everything under a single banner of “ulcer”. That simplification obscures a critical point. A dendritic ulcer behaves differently, relapses differently, and can damage vision in ways a bacterial ulcer does not. In this explainer, I set out the causes, risks, warning signs, prevention, and long-term management for herpes eye infection that presents with the classic branching epithelial defect. The goal is simple. Clarity that translates into earlier recognition, safer treatment, and fewer recurrences.
Primary Causes and Risk Factors of Dendritic Ulcers
Herpes Simplex Virus Type 1 Infection
I start with first principles. A dendritic ulcer on the cornea most commonly results from reactivation of herpes simplex virus type 1 in the ophthalmic division of the trigeminal nerve. The virus establishes latency after a primary mucocutaneous infection and later reactivates in corneal epithelium. The outcome is an arborising epithelial defect with terminal bulbs that stains with fluorescein. That pattern is the clinical fingerprint of HSV epithelial disease.
In practice, herpes simplex keratitis varies in depth and immune involvement. A purely epithelial dendritic ulcer differs from geographic ulcers and from stromal keratitis. Stromal disease often follows repeated episodes or immune dysregulation and threatens vision through scarring. The distinction matters because topical steroids may help stromal inflammation yet harm untreated epithelial disease. Wrong drug at the wrong time, and the situation deteriorates quickly.
A quick example underscores the point. A patient with recurrent cold sores develops unilateral redness and photophobia after a cold. An urgent slit lamp exam shows a branching epithelial lesion with terminal bulbs. That is a dendritic ulcer until proven otherwise. I treat with antivirals promptly and avoid topical steroids unless epithelial healing is documented.
Triggers for HSV Reactivation in the Eye
Reactivation is multifactorial. As Herpes Simplex Keratitis – StatPearls – NCBI Bookshelf notes, fever, local trauma, immunosuppression, hormonal shifts, and ultraviolet exposure can precipitate ocular episodes. The shared mechanism is stress on neuronal or local immune control that permits viral replication in the cornea.
Psychological stress also correlates with flares. The link is likely mediated through neuroendocrine pathways that alter immune surveillance in the ocular surface. Surgical trauma near the eye and periocular procedures can occasionally trigger an episode when prophylaxis is not used. Long days on snow or water, with high UV reflection, often precede springtime recurrences. It is predictable enough that I pre-empt with behavioural advice and, in some cases, short antiviral cover.
Thermal shifts and febrile illness also matter. A viral upper respiratory infection may be the final nudge that turns latent HSV back on. That is why a measured winter approach to exposure and rest helps reduce risk in those with frequent relapses.
Immunosuppression and Systemic Conditions
The host response shapes severity. As Herpes Simplex Keratitis – StatPearls – NCBI Bookshelf describes, immunocompromised states increase frequency and intensity of ocular HSV episodes. Chemotherapy, systemic steroids, advanced diabetes, malnutrition, and HIV can all reduce corneal immune control to an extent that minor triggers become major events. In these contexts, a dendritic ulcer can progress to larger geographic defects, neurotrophic epitheliopathy, or stromal keratitis.
There is also an immunological paradox. Suppressing an overactive response can mitigate stromal inflammation, yet broad immunosuppression increases viral replication risk. Management therefore requires calibrated dosing and clear staging. I avoid topical steroids until I am confident the epithelium is intact or the epithelial infection is fully suppressed with antivirals. Timing and sequence are decisive here.
Environmental and Physical Trauma Factors
Environmental load is not trivial. Bright UV exposure, desiccating wind, and low humidity destabilise the tear film and stress epithelial cells. Contact lens overwear adds microtrauma and hypoxia. Mechanical abrasion, even mild, can unmask viral activity in a previously quiescent cornea. I advise patients who ski, sail, or weld to use proper eye protection and strict lubrication routines. The aim is to reduce triggers that tilt the balance toward viral reactivation.
Practical steps help. Wraparound sunglasses with UV400 filtration, frequent preservative-free lubricants during flights, and protective goggles during yard work reduce epithelial stress. None of this guarantees prevention. It lowers the odds in a meaningful way.
Age-Related Risk Factors Across Different Groups
Age modifies both susceptibility and outcome. As Infectious Keratitis in Patients Over 65: A Review on Treatment… highlights, older adults have diminished corneal sensation, reduced tear quality, and altered immune responses. Collectively, these changes increase infection risk and slow healing. Clinical recovery is often longer and visual outcomes can be worse in the elderly cohort.
Children are not exempt, particularly after contact with active cold sores from caregivers. Their immune systems are still calibrating and may respond unpredictably. That said, timely diagnosis and antiviral therapy usually restore the corneal epithelium without long-term compromise. The pragmatic conclusion is simple. I adjust surveillance and threshold for treatment upward at the extremes of age.
Recognising Corneal Ulcer Symptoms and Clinical Features
Early Warning Signs of Herpes Eye Infection
Early symptoms often mimic routine conjunctivitis. Unilateral redness, gritty discomfort, watering, and mild aching present first. A herpes eye infection then diverges with focal foreign body sensation, light sensitivity, and reduced corneal sensation on gentle testing. A prior history of cold sores is a quiet clue that should raise suspicion.
Intraocular pressure may be normal, yet the eye looks angrier than the discomfort suggests. That dissociation is typical when epithelial nerves are affected. I ask about recent stress, illness, sun exposure, or eye trauma. Those answers frequently connect the dots.
Characteristic Dendritic Pattern Formation
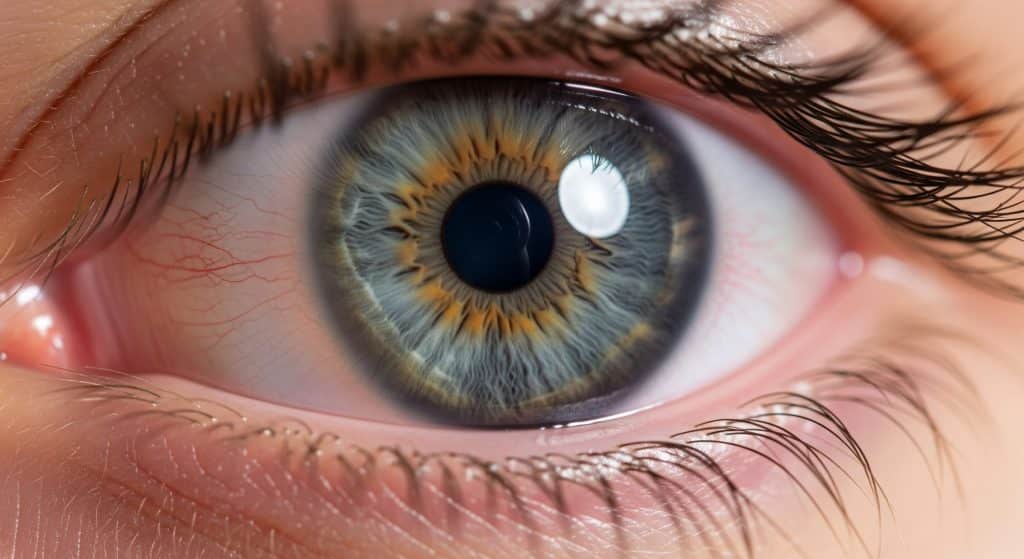
The hallmark is the branching epithelial lesion. I see a central stalk with lateral branches and terminal bulbs at the ends. Fluorescein stains the ulcer bed and Rose Bengal or Lissamine Green can highlight the edges. The appearance is not subtle once seen. It is practically a signature.
In severe cases, the dendritic ulcer coalesces into a geographic ulcer with broader epithelial loss. Recurrent disease can lead to neurotrophic keratopathy, where the cornea loses sensation and epithelial healing stalls. Here is why that matters. A numb cornea does not signal pain properly, so the damage can outpace symptoms.
Visual Changes and Photosensitivity
Vision often blurs due to surface irregularity and tear film instability. Photophobia can be significant, especially with central lesions. Patients describe glare, halos at night, and a film over the eye. When the visual axis is involved, even a small dendritic ulcer can cause disproportionate blur.
Corneal nerves drive tear reflex and blink patterns. When HSV inflames or damages these fibres, dry spots and epithelial punctate staining worsen. The result is more glare and variable acuity through the day. It is basically a cycle that feeds itself until the epithelium heals.
Differentiation from Other Corneal Conditions
Distinguishing HSV from bacterial keratitis, fungal disease, or Acanthamoeba matters for therapy. Bacterial ulcers often have dense infiltrates, overlying epithelial defects, and purulent discharge. Fungal lesions may show feathery margins and satellite lesions. Acanthamoeba presents with severe pain and perineural infiltrates, especially in contact lens wearers.
Epithelial HSV typically shows a clean dendritic pattern without heavy stromal infiltrate early on. Corneal anaesthesia is a helpful sign. I also consider varicella zoster if the rash follows a dermatomal pattern on the forehead or nose. Clinical context plus slit lamp findings guides me away from misdiagnosis.
Prevention Strategies for Herpes Simplex Keratitis
1. Primary Prevention in Uninfected Individuals
Primary prevention focuses on reducing exposure and building resilience. Avoid touching active cold sores. Avoid sharing eye make-up, towels, or contact lenses. Wash hands after contact with facial lesions. These steps reduce inoculation risk to the ocular surface.
I also emphasise UV protection, hydration, and adequate sleep. Healthy tear film and intact epithelium are natural defences against a potential inoculum. While primary ocular HSV remains uncommon, the consequences of first infection can be significant. A cautious routine is therefore justified.
2. Secondary Prevention After Initial Infection
Secondary prevention is where most benefit resides. I review personal triggers with each patient and build a plan around them. For frequent recurrences, daily oral antiviral prophylaxis over months can cut relapse risk substantially. The strategy is iterative and pragmatic.
I also teach early recognition. If the eye begins to sting, water, and dislike light on one side, call early. Starting treatment within the first 24 hours often keeps a small dendritic ulcer from expanding into a geographic lesion. Timing, again, is critical.
3. Lifestyle Modifications and Trigger Avoidance
Practical adjustments prevent many flares:
-
Limit intense midday sun and wear wraparound UV-protective eyewear.
-
Use preservative-free lubricants during flights, outdoor activities, or long screen sessions.
-
Manage stress with structured routines and recovery periods.
-
Avoid ocular surface trauma including aggressive eye rubbing.
-
Pause contact lens wear during minor eye irritation or illness.
Small changes compound. And yet, lapses happen. The aim is not perfection. It is risk reduction week after week.
4. Prophylactic Antiviral Therapy Guidelines
Prophylaxis is considered for patients with recurrent disease, post-keratoplasty risk, or anticipated triggers such as refractive surgery. Typical regimens use oral aciclovir or valaciclovir at suppressive doses. I tailor the dose to recurrence history and renal function. The concept is straightforward. Keep viral replication below a clinical threshold.
For planned ocular surgery in a patient with prior HSV, I initiate oral antivirals in advance and continue through early healing. If there is any epithelial break, I delay surgery until the surface is stable. It is a conservative approach that preserves the graft or flap and reduces the risk of postoperative reactivation.
5. Eye Protection and Hygiene Practices
Hygiene protocols support prevention and shorten active episodes:
-
Do not touch the fellow eye after contacting the affected eye.
-
Discard contaminated contact lenses and cases after an episode.
-
Use separate towels and pillowcases during active disease.
-
Clean glasses frames and work goggles regularly.
-
Follow the 20-20-20 rule to reduce digital eye strain and blinking reduction.
These measures are low cost and high impact. They also reduce transmission risk to household members, especially children.
6. Nutritional Support and Immune System Strengthening
Nutrition does not replace antivirals. It supports epithelial healing and immune balance. I advise adequate protein, omega-3 fatty acids, and micronutrients such as vitamin A and zinc. Hydration matters for tear film quality. Moderate exercise and consistent sleep help regulate inflammatory signalling.
There is no miracle supplement for HSV. Balanced inputs and reduced physiological stress keep the corneal surface more resilient. That resilience buys time until the next challenge.
Treatment Approaches and Long-term Management
Immediate Medical Interventions
Timing determines outcome. I confirm the diagnosis with slit lamp examination and fluorescein staining. If I see a dendritic ulcer, I start antiviral therapy the same day. I educate the patient to stop contact lens wear and to avoid topical anaesthetics. I document corneal sensation and consider baseline intraocular pressure.
If there is suspicion of bacterial coinfection, I consider coverage while awaiting response. Severe pain out of proportion to signs prompts a recheck for Acanthamoeba or herpetic neuralgia. When in doubt, I reassess within 24 to 48 hours. The cornea changes rapidly under active infection.
Antiviral Medications and Dosing Protocols
Topical and oral antivirals form the core. Topical options include ganciclovir gel. Oral agents include aciclovir and valaciclovir. I select based on severity, adherence likelihood, and side effect profile. For epithelial disease, I avoid topical steroids until re-epithelialisation is evident.
In stromal disease with intact epithelium, I add topical corticosteroids under antiviral cover and taper carefully. The taper is slow and deliberate to prevent rebound inflammation. If neurotrophic keratopathy develops, I pivot to surface rehabilitation rather than escalation of anti-inflammatory therapy.
Supportive Care During Active Episodes
Support reduces pain and speeds recovery. I recommend frequent preservative-free lubricants, cold compresses, and appropriate analgesia. For blepharitis or meibomian gland dysfunction, I add lid hygiene to stabilise the tear film. In severe photophobia, temporary tint or a patch for short rest periods may help.
For contact lens users, I hold lenses until full healing and a symptom-free interval has passed. I then reintroduce daily disposable lenses with strict hygiene. Recurrent wearers benefit from a refit and a review of wear schedules. The safest lens is a clean lens worn for the shortest necessary time.
Monitoring for Complications
Complications can escalate quietly. Persistent epithelial defects suggest neurotrophic keratopathy. New stromal haze signals immune activation. Elevated pressure can accompany herpetic uveitis. I monitor with slit lamp exams, staining patterns, and intraocular pressure measurements.
Red flags include reduced corneal sensation, enlarging epithelial defects, or marked anterior chamber reaction. In these cases, I adjust therapy quickly and consider referral to a corneal specialist. A timely second opinion prevents long-term scarring and vision loss.
Recurrence Prevention Strategies
Prevention is a programme, not a pill. I combine trigger management, lubrication routines, UV protection, and periodic prophylaxis. For frequent relapses, I consider low-dose oral antivirals for several months, then reassess. If surgery is planned, I map perioperative antiviral cover with the surgeon.
Education closes the loop. Patients who recognise the earliest tingle and light sensitivity present sooner and heal faster. That behavioural shift reduces both duration and depth of each dendritic ulcer. Fewer flares mean less cumulative nerve damage and better long-term vision.
Conclusion
A dendritic ulcer is not just another corneal scratch. It represents active HSV on a delicate, innervated surface where scars matter. The essentials are clear. Identify the branching lesion early, treat decisively with antivirals, protect the epithelium, and avoid steroids until the surface is closed. Then focus on triggers, hygiene, and targeted prophylaxis to prevent the next episode.
The contrarian take is simple. Prevention deserves more attention than escalation. Small, consistent actions reduce reactivation pressure and protect vision more reliably than any late rescue. That is the discipline that keeps eyes clear and patients confident.
Frequently Asked Questions
Can dendritic ulcers heal completely without scarring?
Yes, many epithelial lesions heal without scarring when treated promptly. The corneal surface remodels well if the infection remains superficial. Risk rises with delayed therapy, central location, large geographic expansion, and repeated episodes. Stromal involvement is the main driver of permanent opacity. Quick antiviral treatment and careful surface care improve the odds of a clear result.
How long does a herpes eye infection typically last?
Uncomplicated epithelial disease usually improves within a few days and re-epithelialises over one to two weeks. Vision and comfort then stabilise. Recovery can take longer with neurotrophic changes or stromal inflammation. Early presentation shortens the course. Late recognition prolongs it and increases the chance of a larger dendritic ulcer.
Is dendritic ulcer contagious to other people?
The lesion itself is a manifestation of HSV in the cornea. The virus can spread through direct contact with eye secretions during active disease. Hand hygiene and separate towels are prudent until the surface heals. Household transmission is uncommon with basic precautions. Avoid touching the other eye after treating the affected side.
What percentage of people with oral herpes develop eye infections?
Only a minority develop ocular disease. Most individuals with oral HSV never experience an eye complication. Risk rises with known triggers, immunosuppression, and prior ocular episodes. From a practical standpoint, vigilance matters most in those with a previous dendritic ulcer or frequent cold sores.
Can children get dendritic ulcers from cold sores?
Yes, children can acquire ocular HSV through contact with active cold sores, usually from close caregivers. Hygiene and avoiding facial contact during active lesions reduce this risk. If a child presents with unilateral redness, tearing, and light sensitivity, I recommend urgent review. Early treatment produces excellent outcomes in most cases.
Are contact lens wearers at higher risk for corneal ulcers?
Contact lens wear increases the risk of corneal infections in general due to hypoxia, microtrauma, and contamination. For HSV, lenses can exacerbate surface stress and delay healing during active disease. I advise immediate discontinuation during any episode and a cautious reintroduction later. Daily disposables, strict hygiene, and reduced wear time lower future risk.
Quick Reference: Key Terms
|
Term |
Definition |
|---|---|
|
Dendritic ulcer |
A branching corneal epithelial defect with terminal bulbs, typical of HSV epithelial disease. |
|
Herpes simplex keratitis |
Corneal inflammation caused by HSV, ranging from epithelial to stromal involvement. |
|
Neurotrophic keratopathy |
Corneal disease from reduced corneal sensation leading to poor epithelial healing. |
|
IOP |
Intraocular pressure, monitored to detect pressure spikes during uveitic episodes. |
|
SPK |
Superficial punctate keratitis, fine epithelial staining that reflects surface stress. |
Clinical Pattern Checklist
-
Unilateral redness and photophobia after stress, illness, or UV exposure.
-
Reduced corneal sensation compared with the fellow eye.
-
Branching epithelial lesion with terminal bulbs on staining.
-
Rapid response to antivirals in epithelial disease.
-
Delay steroids until epithelium heals or is protected by antivirals.
When to Seek Urgent Care
-
Sudden unilateral light sensitivity and blurred vision, especially with a history of cold sores.
-
Central lesion, severe pain, or worsening symptoms despite initial care.
-
Signs of deeper involvement such as stromal haze or marked inflammation.
-
Any ocular symptoms in immunosuppressed patients or after eye surgery.
Early review prevents complications. That is the leverage point that protects sight.
Putting It All Together
Cause, trigger, surface integrity, and host immunity determine the appearance and course of a dendritic ulcer. Recognise the branching pattern early. Treat with antivirals promptly. Stabilise the surface. Then remove as many reactivation cues as possible. It is disciplined rather than dramatic.
I also keep the language clear for patients. A dendritic ulcer is an HSV flare on the cornea. It is contagious through secretions, not through casual conversation. It needs antivirals, not steroid drops at the outset. And most heal well when treatment starts early.
Contextual Notes on Patterns and Keywords
Clinically, the term dendritic ulcer should be reserved for the epithelial branching lesion seen in herpes eye infection. Wider geographic ulcers and stromal disease represent a different phase of herpes simplex keratitis. For readers scanning for corneal ulcer symptoms, the triad of unilateral redness, light sensitivity, and foreign body sensation is a strong early combination. When that cluster follows stress or UV exposure, I maintain a high index of suspicion.







 We do what's right for you...
We do what's right for you...








